Insurance fraud is a serious and growing issue that affects both individuals and organizations within the insurance industry. It involves deceptive practices aimed at obtaining financial gain through false or exaggerated claims. While some cases involve large-scale criminal operations, others stem from everyday policyholders misrepresenting facts. Regardless of scale, insurance fraud increases costs, erodes trust, and places an unnecessary burden on honest policyholders and insurance providers alike. Understanding what insurance fraud is and how it impacts everyone involved is crucial to fostering a more transparent and fair insurance system.
What is Insurance Fraud?
Insurance fraud refers to any deliberate act of deception committed to secure an unfair or unlawful financial benefit from an insurance process. It can occur at various stages of the insurance cycle—from application to claims settlement—and may involve policyholders, third parties, or even professionals within the industry. There are generally two categories: hard fraud, which includes planned or staged events like fake accidents or thefts, and soft fraud, which involves exaggerating legitimate claims or omitting relevant information. Both types undermine the integrity of the insurance system and contribute to increased premiums and operational costs.
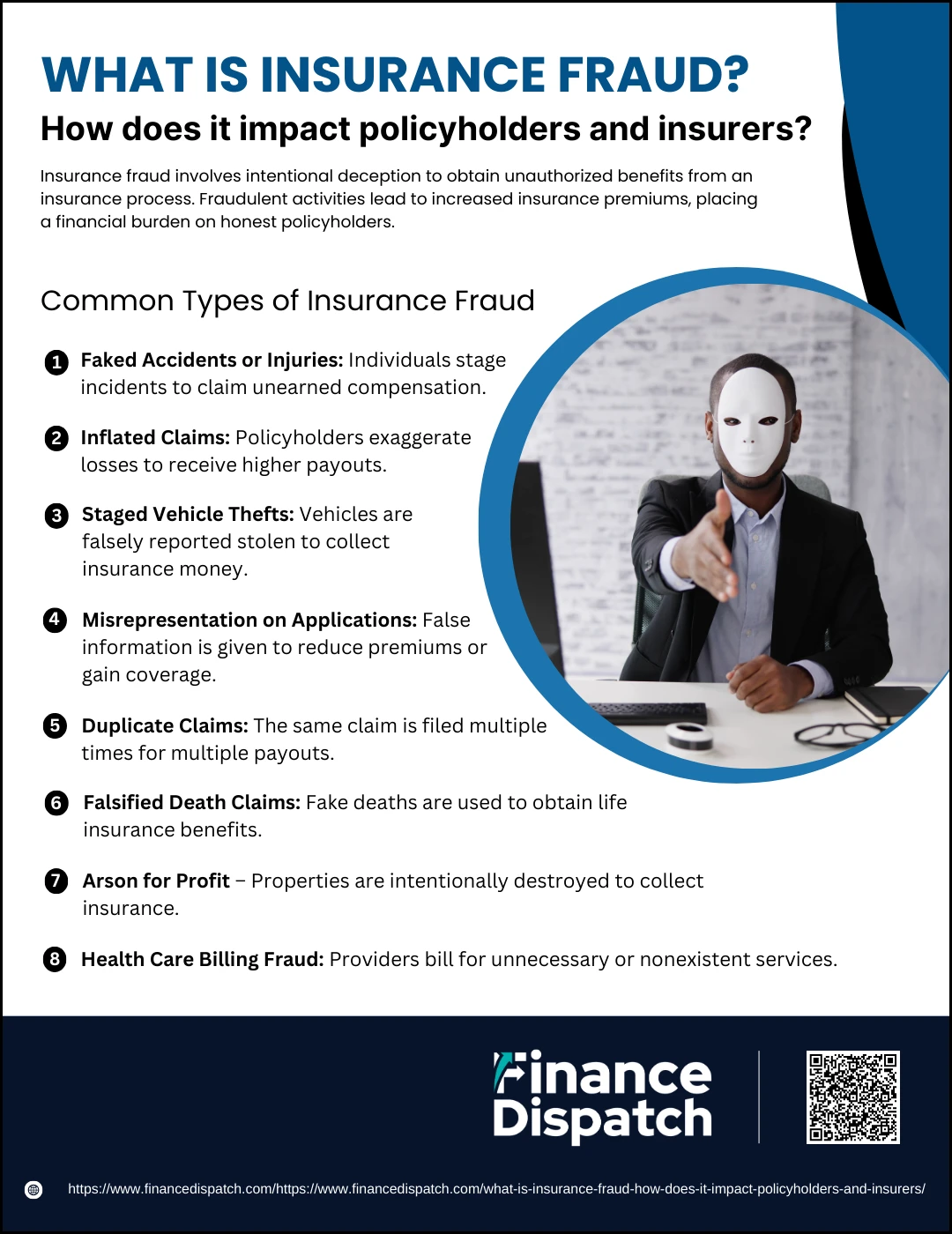 Common Types of Insurance Fraud
Common Types of Insurance Fraud
Insurance fraud takes on many forms and can be committed by individuals, organized groups, or even professionals within the system. While some acts of fraud are carefully planned and executed, others are subtle, involving small exaggerations or omissions. Whether minor or severe, these fraudulent activities cost the industry billions each year and directly impact honest policyholders by driving up premiums and reducing trust in the system. Here are some of the most frequent types of insurance fraud seen across different sectors:
1. Faked Accidents or Injuries
Fraudsters may stage car crashes, slip-and-fall incidents, or fake injuries in order to claim compensation for medical treatment, lost wages, or pain and suffering that never occurred.
2. Inflated Claims
This common type of soft fraud involves exaggerating the extent of damage or loss—for example, claiming a higher repair cost for a damaged item or listing extra stolen goods that were never taken.
3. Staged Vehicle Thefts
Policyholders may arrange for someone to “steal” their car or hide it themselves, then report it as stolen to collect a payout from their auto insurance.
4. Misrepresentation on Applications
Providing false information when applying for a policy—such as underreporting risky behavior, omitting medical conditions, or falsifying a driving record—can lead to lower premiums or approval for coverage that would otherwise be denied.
5. Duplicate Claims
In this scheme, the same damage or loss is reported to multiple insurers or submitted repeatedly to the same insurer under different policies in an attempt to receive multiple payments.
6. Falsified Death Claims
Some individuals fake their own death or that of a relative, using forged documents to claim life insurance benefits. These cases often involve coordinated efforts and fake identities.
7. Arson for Profit
Property owners may deliberately set fire to their buildings, homes, or vehicles and then file claims for the “accidental” loss, often trying to collect more than the actual value of the property.
8. Health Care Billing Fraud
Healthcare providers may submit inflated bills, charge for procedures never performed, or upcode services to receive higher reimbursements from insurance companies.
Real-Life Examples of Insurance Fraud
Understanding real-world cases of insurance fraud helps illustrate how these schemes operate and the consequences they carry. These examples, drawn from various sectors like auto, health, and life insurance, show that fraud can range from minor exaggerations to complex, criminal conspiracies. Authorities around the world regularly investigate and prosecute such frauds, emphasizing the seriousness of these offenses.
1. The Staged Auto Accident Ring (USA) – In Florida, a group staged car crashes and sent fake patients to clinics that billed insurers for non-existent injuries and treatments, resulting in millions in fraudulent claims.
2. Fake Death for Life Insurance (India) – A man faked his own death using a burned body of another person to claim a ₹15 lakh life insurance policy. He was caught when inconsistencies in documents raised red flags.
3. Arson for Profit (United Kingdom) – A business owner set fire to his own restaurant and filed a claim for over £200,000, claiming an electrical fault. Investigators discovered traces of accelerants and deliberate tampering.
4. Health Insurance Billing Scam (USA) – A clinic owner in California was charged with billing Medicare for over $10 million in services that were never provided, including ghost surgeries and false prescriptions.
5. Luxury Car Dumping (Canada) – Several owners of expensive vehicles, facing loan defaults, reported their cars stolen. Investigations found the vehicles had been sold overseas or dumped in lakes and ravines.
6. False Injury Claims in Slip-and-Fall (USA) – A woman deliberately spilled water on a store floor, pretended to slip, and filed a claim for back injuries. Surveillance footage revealed her actions, leading to her arrest.
7. Multiple Policy Payouts (South Africa) – A man insured his wife with multiple companies and then murdered her to collect payouts. The fraud was uncovered during police investigation due to overlapping policies and suspicious timing.
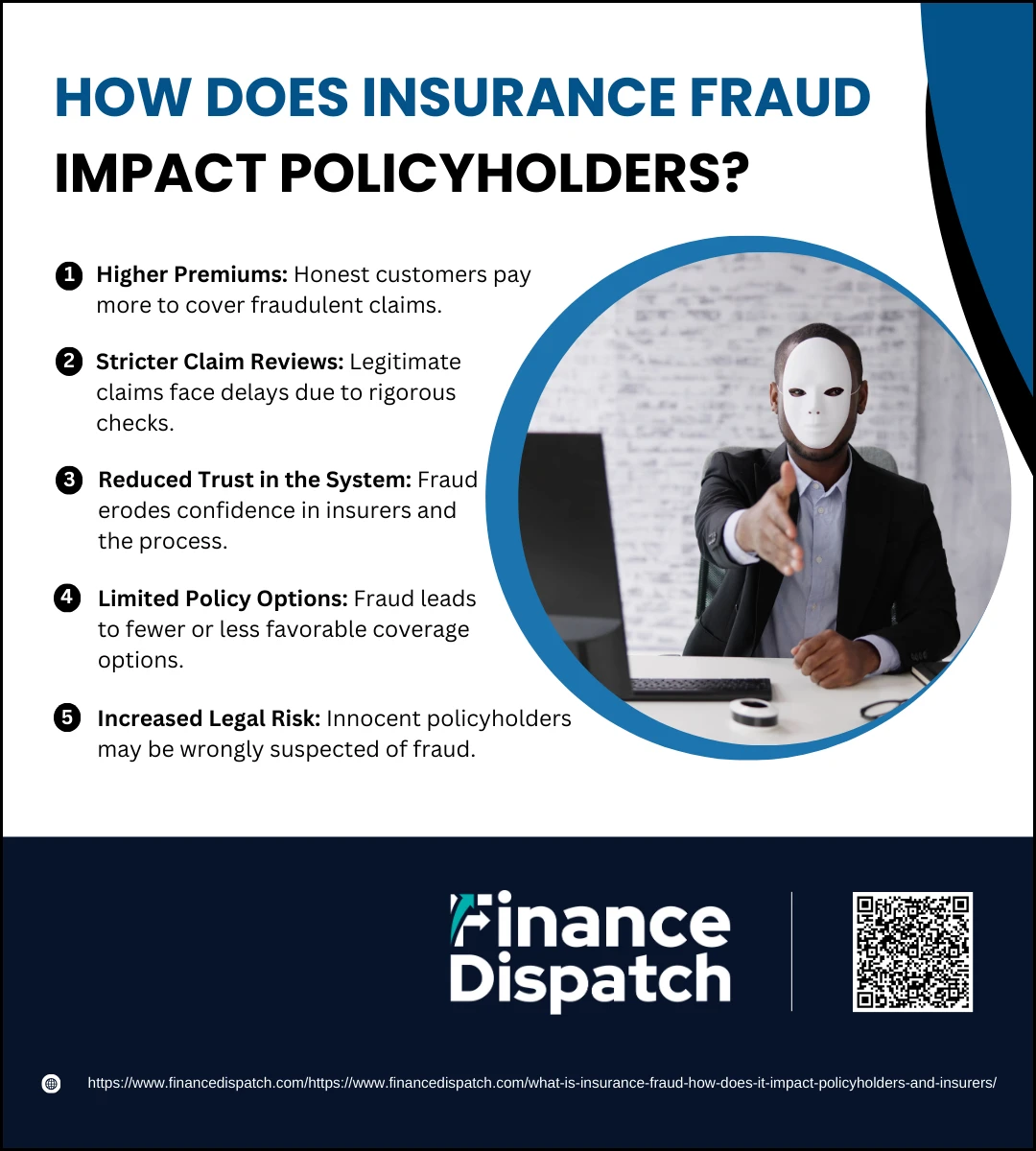 How Does Insurance Fraud Impact Policyholders?
How Does Insurance Fraud Impact Policyholders?
Insurance fraud may seem like a crime committed against large corporations, but its consequences fall heavily on everyday policyholders. When someone cheats the system, the financial burden doesn’t just stay with the insurer—it gets passed on to the broader customer base. Honest individuals end up paying the price in the form of higher premiums, more complicated claims processes, and reduced service quality. In the long run, fraud creates a less efficient and less trustworthy insurance system for everyone.
1. Higher Premiums
One of the most direct consequences of insurance fraud is the increase in insurance premiums for honest customers. To cover fraudulent losses, insurance companies adjust their pricing models, spreading the extra costs across their entire customer base. This means that even policyholders who have never filed a claim may end up paying significantly more over time.
2. Stricter Claim Reviews
To combat fraud, insurers adopt more rigorous verification procedures. This includes thorough background checks, extra documentation, and extended evaluation periods. While these steps are designed to protect against fraud, they also lead to delays and frustrations for genuine claimants.
3. Reduced Trust in the System
When fraud becomes widespread, policyholders start to lose faith in their insurance providers. Doubts may arise about whether claims will be paid fairly and on time, or whether innocent mistakes could be treated as fraud. This erosion of trust affects the relationship between insurer and customer.
4. Limited Policy Options
As fraud risk increases, insurers often respond by tightening coverage terms, increasing deductibles, or even pulling certain products from the market. Policyholders are then left with fewer options or less comprehensive coverage, even if they have a clean record.
5. Increased Legal Risk
In some cases, honest policyholders may be wrongly flagged for suspicious activity due to fraud detection software. This can result in time-consuming investigations, withheld claim payments, or even legal trouble—despite having done nothing wrong. Such experiences can be stressful and financially damaging.
 How Does Insurance Fraud Affect Insurers?
How Does Insurance Fraud Affect Insurers?
Insurance fraud is not just a nuisance—it’s a serious threat to the financial health and operational efficiency of insurance companies. Every fraudulent claim, whether it’s staged, exaggerated, or completely fabricated, places added strain on insurers. To stay afloat and continue offering services, insurers must implement costly fraud detection measures, increase prices, and sometimes even scale back on coverage options. These consequences create a ripple effect, changing how insurers do business and how they are perceived by customers and regulators.
1. Financial Losses
Fraudulent claims significantly reduce insurers’ profit margins. It’s estimated that billions of dollars are lost each year globally due to fraud. These losses directly impact an insurer’s ability to remain competitive and financially stable, especially in high-risk sectors like auto, health, and property insurance.
2. Increased Operational Costs
Detecting and preventing fraud is expensive. Insurers must hire fraud investigators, invest in artificial intelligence tools, and provide ongoing training for staff. These additional operating costs strain resources and reduce funds available for improving services or innovating new products.
3. Longer Claim Processing Times
As insurers become more cautious, they introduce more layers of claim verification. While these steps help catch fraudulent claims, they also slow down the process for genuine customers, resulting in delays and dissatisfaction.
4. Reputational Damage
When an insurer becomes associated with high rates of fraud—especially if high-profile cases go public—it can lose the trust of current and potential clients. This loss of credibility may also drive customers toward competitors, affecting long-term growth.
5. Regulatory Scrutiny and Legal Issues
Insurance companies operating in fraud-prone markets may face closer examination by regulators. This could lead to fines, audits, and additional compliance requirements, all of which increase the administrative burden and reduce flexibility.
6. Product and Pricing Adjustments
To recover from losses, insurers often raise premiums, tighten underwriting policies, or limit benefits. While necessary from a business standpoint, these changes can make insurance products less appealing and drive customers to seek alternatives.
Statistics on Insurance Fraud
Insurance fraud continues to be a major concern for the global insurance industry, with billions of dollars lost each year to dishonest claims and criminal activity. These losses affect not only insurers but also policyholders, regulators, and the economy as a whole. To better understand the scope of the problem, let’s look at some key statistics from recent years, focusing on estimated losses, most affected sectors, and fraud’s share of total claims.
| Year | Estimated Fraud Loss (U.S.) | Most Affected Sector | % of Total Claims Affected by Fraud |
| 2020 | $40 Billion | Health Insurance | 10% |
| 2021 | $42 Billion | Auto Insurance | 9% |
| 2022 | $45 Billion | Life Insurance | 11% |
| 2023 | $48 Billion | Property Insurance | 12% |
| 2024 | $50 Billion (Projected) | Mixed Lines | 13% |
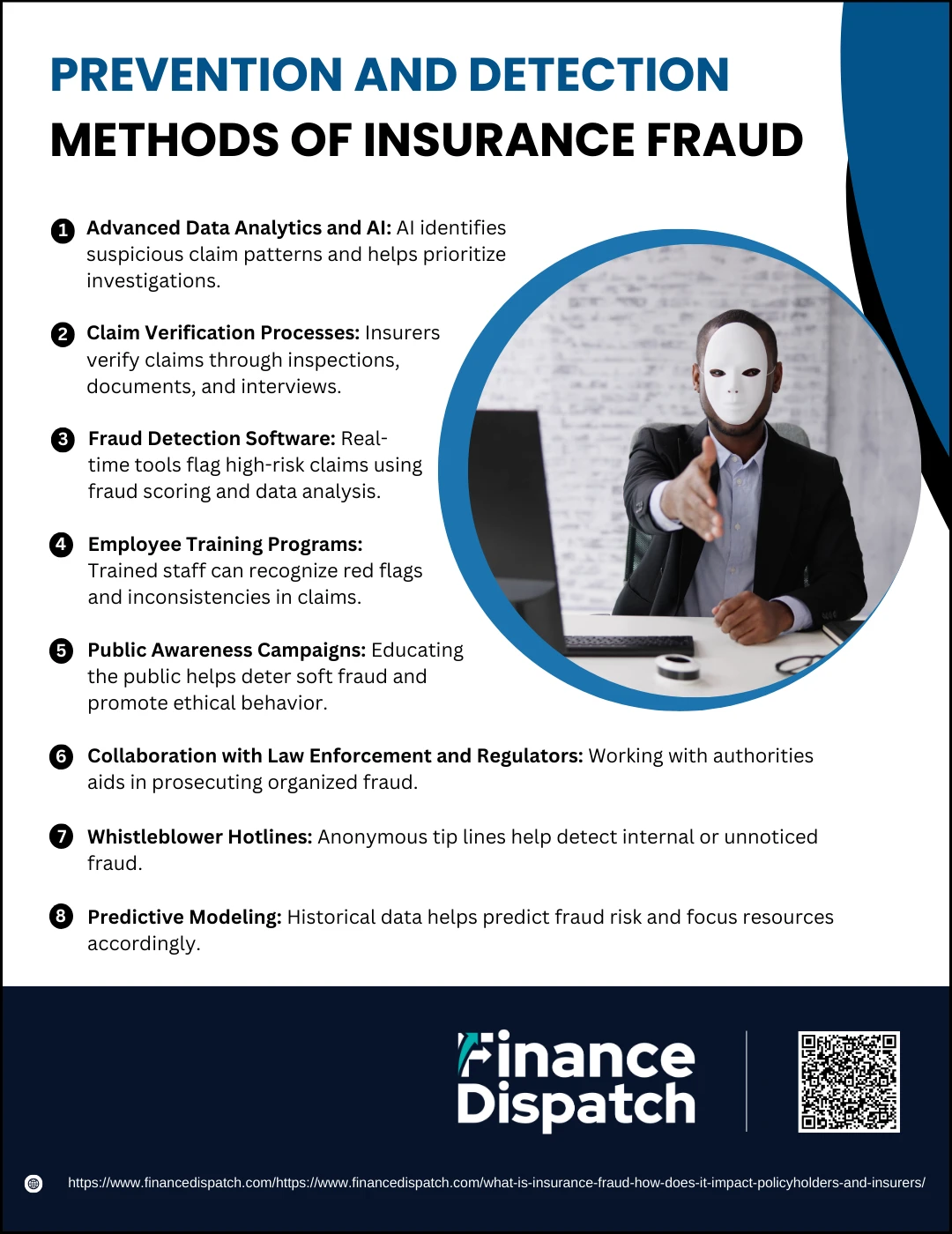 Prevention and Detection Methods of Insurance Fraud
Prevention and Detection Methods of Insurance Fraud
Insurance fraud continues to evolve, often becoming more difficult to detect as fraudsters use increasingly advanced tactics. To stay ahead, insurance companies must invest in both technology and human expertise. Prevention is just as crucial as detection—by stopping fraud before it happens, insurers can save time, money, and resources. A comprehensive approach combines analytics, training, public education, and collaboration with authorities. The goal is to maintain the integrity of the insurance system and ensure that honest policyholders are not penalized for the actions of a few.
1. Advanced Data Analytics and AI
Insurers leverage artificial intelligence and big data to identify unusual patterns in claims, such as repeated use of the same repair shops or identical accident descriptions across multiple claims. These systems continuously learn and adapt, improving their accuracy over time and helping investigators prioritize the most suspicious cases.
2. Claim Verification Processes
Manual and automated checks are used to validate the accuracy of claim information. This may involve requesting receipts, interviewing claimants, inspecting damaged property, or even using satellite imagery in cases of natural disaster claims. These steps reduce the chances of fake or exaggerated claims going undetected.
3. Fraud Detection Software
Tools such as fraud scoring systems analyze claim details in real time, flagging them based on their likelihood of being fraudulent. These tools use data from internal records and external sources, including national fraud databases, to identify known fraud patterns and suspicious activity.
4. Employee Training Programs
Staff who handle claims are often the first line of defense. With proper training, they can spot red flags such as inconsistencies in statements, unusual timing, or aggressive behavior from claimants. Regular workshops and updated guidelines help maintain a high level of awareness.
5. Public Awareness Campaigns
Educating the public about the legal consequences and ethical concerns of insurance fraud can discourage “soft fraud,” which involves small misrepresentations by everyday people. Campaigns may include social media posts, advertisements, or newsletters highlighting real fraud cases and their outcomes.
6. Collaboration with Law Enforcement and Regulators
Insurance companies often cooperate with law enforcement agencies, fraud bureaus, and regulatory bodies to pursue criminal charges against serious offenders. Sharing data and intelligence strengthens the fight against organized fraud rings and enables more successful prosecutions.
7. Whistleblower Hotlines
Many insurers establish secure, anonymous tip lines that allow employees, customers, and third parties to report suspicious activity. These tips can be a valuable source of information that may otherwise go unnoticed, especially in internal fraud cases.
8. Predictive Modeling
By analyzing historical fraud data, insurers develop models that forecast the probability of fraud in new claims. These models allow insurers to allocate resources more effectively, focusing attention on high-risk claims without delaying genuine ones.
 Legal Consequences of Committing Insurance Fraud
Legal Consequences of Committing Insurance Fraud
Committing insurance fraud carries serious legal implications that extend far beyond paying back the stolen funds. Because fraud undermines the integrity of the entire insurance system and affects millions of honest policyholders, it is treated as a criminal offense in most jurisdictions. Whether committed by an individual faking an injury or an organized group staging multiple claims, fraud is aggressively prosecuted. Penalties are designed to be harsh to serve as a deterrent, and the consequences can affect every aspect of an offender’s personal, financial, and professional life.
1. Criminal Charges
Insurance fraud is a punishable crime under both state and federal law. Offenders may be charged with various offenses, including fraud, identity theft, falsification of documents, mail fraud, and conspiracy. These charges are often stacked, especially in organized schemes, leading to more severe penalties.
2. Imprisonment
Depending on the severity of the fraud, individuals may receive prison sentences ranging from several months to over a decade. For instance, large-scale fraud involving millions of dollars or harm to others often results in longer sentences. Courts also take prior offenses into account when determining the sentence.
3. Heavy Fines
Financial penalties are commonly imposed alongside or instead of prison time. These fines are meant to recover damages and penalize the offender. They can range from thousands to millions of dollars, particularly in cases involving significant financial loss or fraudulent billing schemes.
4. Restitution Orders
Courts often require convicted fraudsters to pay restitution to the affected insurance companies or policyholders. This repayment may include the full amount of the false claim plus interest and legal costs, placing a long-term financial burden on the offender.
5. Civil Lawsuits
Apart from criminal proceedings, insurance companies may file civil suits to recover additional damages, especially if the fraud caused reputational harm or operational disruption. Civil cases can lead to asset seizures, liens, and wage garnishment.
6. Loss of Insurance Coverage
Once convicted of fraud, individuals typically lose their existing insurance policies. Future attempts to obtain coverage are often denied or approved only at much higher premiums, limiting access to basic protections like health, auto, or life insurance.
7. Criminal Record
A conviction for insurance fraud becomes part of the offender’s permanent criminal record. This can hinder job prospects, prevent travel to certain countries, disqualify individuals from obtaining loans, and damage long-term financial stability.
8. Professional Consequences
Professionals such as doctors, attorneys, insurance agents, and contractors involved in fraud may face disciplinary action from licensing boards. This could include suspension or permanent revocation of their licenses, effectively ending their careers.
9. Increased Regulatory Oversight
Insurance companies or brokers caught engaging in fraud may be subjected to audits, closer monitoring, and heavy fines by regulatory agencies. In extreme cases, their business licenses can be suspended or revoked, disrupting their entire operations.
Conclusion
Insurance fraud is a widespread and costly issue that affects everyone—from insurers and policyholders to regulators and service providers. While fraudsters may see it as a quick way to gain money, the long-term consequences are severe, both legally and ethically. For insurers, it leads to financial strain, increased operational costs, and a loss of customer trust. For honest policyholders, it results in higher premiums, stricter claim procedures, and fewer coverage options. Combating insurance fraud requires a collective effort that includes advanced detection methods, public awareness, strong legal enforcement, and a commitment to integrity at every level of the industry. By understanding and addressing insurance fraud, we can work toward a fairer, more transparent insurance system for all.